San Francisco Pays for the Mental Health System the State Dismantled
May 19, 2025
San Francisco bears the cost of a broken mental health system, with insufficient state and federal support for long-term care.
San Francisco is in the middle of a behavioral health crisis that plays out on our streets, in our emergency rooms, and throughout our legal system. At the center of this crisis is a basic infrastructure failure: we don’t have enough treatment beds for people with serious mental illness, and even when beds exist, the people who need them most are often turned away.
This isn’t just a problem of mismanagement or delayed investment. It’s the result of decades of policy decisions at the state and federal levels that have left cities like San Francisco holding the bag. We now have to fund, staff, and operate complex systems of care that were once the responsibility of the State.
“The overrepresentation of severely mentally ill people on our streets… is the legacy of de-institutionalization and the State’s failure to make good on the promise to find a better alternative.”
– Supervisor Rafael Mandelman, Letter in Report, p. 3
This report explains how we got here, what’s missing, and why San Francisco is paying the full cost of care for a system it didn’t design and can’t sustain alone.
What the State used to provide, the city now has to
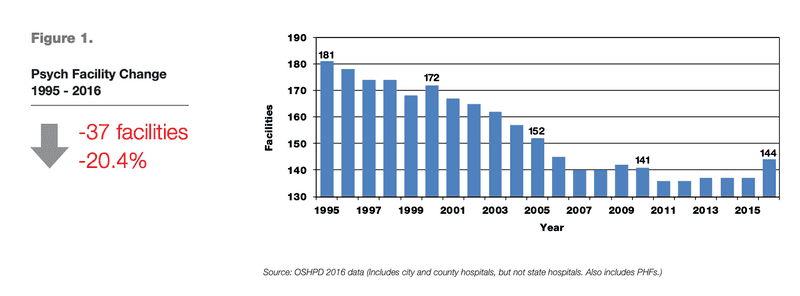
Source: California Psychiatric Bed Annual Report, p. 5
What we now call “deinstitutionalization” began in the 1950s and 1960s, when California shut down the majority of its state hospitals. This shift was driven by several factors: the emergence of psychotropic medications that reduced the need for long-term institutionalization, widespread reports of inhumane conditions inside state facilities, and a push for cost savings at the state level.
At its peak in the 1950s, California’s state hospital system operated approximately 37,000 beds. By June 2024, that number had dropped to just 5,724 — a decline of 85%. Meanwhile, California’s population has more than doubled, from under 16 million in 1960 to nearly 39 million today. Had the number of state hospital beds kept pace with population growth, California would have around 90,000 beds today — nearly 16 times more than currently exist.
As the State retreated, cities were forced to fill the gap with no funding, no infrastructure, and no authority. So many of our challenges housing and treating those with untreated mental illness can be traced back to this decline in State responsibility.
As of 2024, only 22 San Francisco residents are in State hospitals.
Decline in State Responsibility and Shift to Local Burden
| Year | CA state hospital Capacity | CA Population (Millions) | Expected Beds if Scaled | SF Residents in state hospitals | Implication for San Francisco |
|---|---|---|---|---|---|
| 1955 (Peak) | ~37,000 inpatient placements | ~15.8 | N/A | N/A | State system still intact |
| 2024 | 5,724 inpatient placements | ~39 | ~90,000 | 22 | State capacity collapsed; SF forced to build its own system |
Source: Residential Care and Treatment Working Group Final Report (January 2025)
The cherry on top is that there is no single statewide waitlist and no guaranteed slots for entry into the state hospital system.
Federal and state funding don’t pay for the beds we actually need
It might seem reasonable to expect that the State would help fund inpatient placements — or at the very least, that cities wouldn’t have to shoulder the entire cost. But that’s not how the system works.
“The City must cover the cost of expanding and operating… ARF (adult residential facilities), RCF (residential care facilitie)], and MHRC (mental health rehabilitation centers) programs through local funding sources and the General Fund due to current state and federal funding limitations.”
– Residential Care and Treatment Working Group Final Report, page 15
Since 1965, a federal Medicaid policy known as the Institutions for Mental Disease Exclusion (the “IMD Exclusion”) has prohibited the use of federal funds for mental health facilities with more than 16 beds. The original idea was to encourage smaller, community-based care managed at the county level, under the assumption that counties would operate smaller facilities.
Because Medi-Cal follows federal Medicaid rules, neither the state nor the federal government can use public insurance to pay for care in IMDs. This is why Mental Health Rehabilitation Centers (MHRCs) — which exceed 16 beds and are primarily focused on mental health care — are ineligible for reimbursement. Adult Residential Facilities (ARFs) and Residential Care Facilities for the Elderly (RCFEs) do not receive Medicaid funding in California because they are not considered medical facilities at all.
Note, though, that the IMD exclusion does not apply to psychiatric wards within general hospitals. That means Medi-Cal will reimburse general hospitals for short-term acute psychiatric care, even if those hospitals exceed 16 beds. But once the patient is moved to a long term facility (after 7 days, on average), the funding vanishes.
So San Francisco can receive Medi-Cal funding for a short hospital stay, but not for longer-term residential treatment in facilities much better suited for recovery.
Here’s what these facilities look like, and what they cost when cities like San Francisco have to fund them alone:
| Facility Type | # of Beds SF Needs | Federal or State Reimbursable? | Avg. Daily Cost | Avg. Stay | Total SF Cost Per Person |
|---|---|---|---|---|---|
| Mental Health Rehabilitation Centers (MHRCs) | 55-95 | ❌ | $313-$577 (avg: $506) | 2 years | $370,000 |
| Adult Residential Facilities (ARFs) | 20-40 (combined ARFs and RCFs) | ❌ | $46-$250 (avg: $130) | 6.8 years | $372,000 |
| Residential Care Facilities for the Elderly (RCF-Es) | 20-40 (combined ARFs and RCFs) | ❌ | $46-$250 (avg: $111) | 4.4 years | $178,000 |
Source: Residential Care and Treatment Working Group Final Report (January 2025)
The city pays the full cost of long-term treatment
San Francisco is effectively on its own when it comes to funding long-term mental health treatment. The City must place, operate, and pay for care without support from the State – and without access to federal or state operating funds. Treating a single individual with serious behavioral health needs can cost hundreds of thousands of dollars over the course of several years – a worthwhile cost, but one we shouldn't have to bear alone
Unlike many medical services that are reimbursed through Medi-Cal or Medicare, the types of facilities San Francisco needs the most (MHRCs and ARF/RCF-Es) receive no ongoing operational funding from state or federal sources. As a result, the full cost falls on the City’s General Fund.
“San Francisco pays approximately $35 million annually on ARF/RCF-E services, and $26 million on MHRC services—all from the General Fund.”
– Residential Care and Treatment Working Group Final Report, page 17
When we talk about “treatment costs,” we mean everything required to care for someone with high behavioral health needs, including:
- Staffing and clinical labor (including 24/7 care at MHRCs)
- Facility rent, maintenance, and capital improvements
- Food, security, utilities, and day-to-day operations
- Liability coverage, insurance, and regulatory compliance
- Wraparound support services like case management, housing navigation, and transportation
To illustrate the scale of this financial burden, here are examples of the unreimbursed costs San Francisco currently pays for various facility types:
| Facility | Total beds | Annual cost | Funding source |
|---|---|---|---|
| Adult Residential Facilities / Residential Care Facilities for the Elderly (ARF/RCF-E) | 640 | $35M | General Fund |
| Mental Health Rehabilitation Centers (MHRCs) (Estimates) | ~125-150 | Est ~$20M-$30M | General Fund |
Source: Residential Care and Treatment Working Group Final Report (January 2025)
Staffing shortages are undermining the entire system
It’s no surprise that San Francisco’s behavioral health workforce is struggling with both high vacancy and high turnover. These jobs are physically and emotionally demanding, offer uncompetitive pay, and provide limited opportunities for advancement. A city staffing analysis found that Behavioral Health Clinicians in the civil service had an 8.9% resignation rate in 2022–2023, the highest of any classification in the Department of Public Health. Former employees cited burnout from high caseloads, better pay and benefits in private health systems, and long hiring timelines with few promotion pathways as key reasons for leaving.
| Job | Vacancy Rate (FY22-23) | Purpose of Job |
|---|---|---|
| Health worker III staff | 29% | Supports client engagement, care coordination, and outreach. |
| Licensed behavioral health workers (Nonprofit programs) | 20.9% | Provide frontline care in outpatient, residential, and community-based settings. |
| Behavioral Health Clinicians (Civil Service) | 17.5% | Provides therapy, assessments, and clinical treatment. |
| Non-licensed behavioral health workers (Nonprofit programs) | 10.3% | Provides daily living support like bathing, meals, and mobility. |
Source: MHSF Staffing Analysis Report
A UCSF study from February 2023 found that 70% of county behavioral health agencies reported difficulty recruiting licensed mental health and substance use professionals. Across counties in California, staffing shortages are common because of the relatively low wages that mental health treatment organizations offer.
San Francisco has about 2,500 behavioral health beds, but needs more
San Francisco currently has a residential behavioral health bed inventory of 2,551 beds as of FY 2023-2024. This includes:
- Mental Health Residential programs (~1,861 beds as of FY 23-24)
- Includes emergency and acute care, locked residential treatment, voluntary residential treatment, low-threshold MH care, therapeutic residences, residential care facilities, mental health housing
- Substance use residential programs (~690 beds as of FY 23-24)
- SUD residential treatment, low-barrier SUD residential, therapeutic residences, co-ops
But this still falls 200 beds short, and even existing capacity is strained by funding, staffing, and regulatory barriers.
This is a crisis cities were never meant to carry alone
San Francisco is doing what the state and federal governments no longer do: providing long-term, intensive treatment for people with serious mental illness and substance use disorders. But the City is doing it alone without reimbursement, without enough beds, and without a sustainable workforce. While the need is growing, our resources are constrained by outdated funding rules, staffing shortages, and a complete absence of guaranteed state hospital access.
If San Francisco is to meet the needs of its most vulnerable residents – and if we are serious about addressing homelessness, public safety, and the human toll of untreated illness – then we must do more than build local programs. We need a structural fix: one that restores the role of the State in providing care, retools federal funding to match real needs, and enables cities to act with urgency.
Without that, we will continue to triage a crisis that we were never meant to manage alone.
“Counties cannot achieve a sustainable expansion without increased support from the State.”
– Residential Care and Treatment Working Group Final Report, page 8
What you can do
Thanks to the work of Supervisor Rafael Mandelman’s Residential Care and Treatment Working Group, the City now has a concrete target for how many inpatient placements are needed. That’s a critical step forward. But meeting that need will require clear prioritization in upcoming budget cycles even as the City faces a significant deficit.
It will also require difficult decisions about how to allocate limited capacity. San Francisco is a regional hub, and people experiencing untreated mental illness often arrive here from other parts of the state. But if the City is building and funding its own inpatient system in the absence of state support, then it’s reasonable to ask whether local resources should be prioritized for residents of San Francisco.
Other systems do this. In Zurich, for example, behavioral health services are reserved for established residents, and people are referred back to their home jurisdictions to receive care. San Francisco is already moving in this direction: Mayor Daniel Lurie recently updated eligibility for public assistance to include proof of local ties. A similar standard could be applied to long-term behavioral health placements, coupled with expanded support for humane return and care coordination across counties.
But at the end of the day, this is a statewide system failure and it requires a structural response. As new leaders step into office at the state and federal levels, voters should be clear about what’s needed: long-term investment, sustained operations, and political will.
What we need to advocate for:
- Dedicated state and federal funding streams to support the construction and long-term operation of inpatient behavioral health facilities, including Mental Health Rehabilitation Centers and Residential Care Facilities.
- Full implementation of California’s expanded conservatorship laws, with local and state leaders committing to build out the placements, clinical staff, and court infrastructure these laws require.
- A multi-billion dollar capital plan to fund the creation of thousands of new inpatient placements statewide (especially in high-need urban counties) and not just pilot programs or temporary grants. We suspect this may actually save us money in the long-term, given the remarkable costs of letting people ricochet through emergency rooms)
- Legislative and regulatory changes to modernize outdated federal rules like the IMD Exclusion, and to remove local legal barriers that prevent the creation of residential treatment programs at the scale needed.
- Clear residency standards and cross-county coordination to ensure that cities like San Francisco aren’t expected to shoulder the full cost of care for individuals from across the state.
Prop 1 in 2024 was a necessary start. But it was only a start. Building the system that Californians need—staffed, accessible, and built to last—will take much more.
Generate a Personalized Email to the Board of Supervisors
To:
Sign up for the GrowSF Report
Our weekly roundup of news & Insights